The Top 8 Health Insurance Terms to Know When Buying a Plan
Health insurance can easily sound complicated or confusing, and so can the terms that go along with it. Whether you’re someone looking for health insurance or an existing policyholder, we want to give you the keys to understand insurance plans better and feel confident in your choices.

To make sure you are getting the most out of your coverage, it is vital to know how each term relates to your overall plan and what it means for you, your needs, and your budget.
We have prepared a list of common health insurance terms that you might encounter when searching for an insurance plan or using your existing policy.
Premium
A health insurance premium is an amount you pay for health insurance coverage. The amount of your premium depends on your age, the plan you choose, and whether you qualify for any discounts.
The premium is usually higher if you are older and have a higher risk of increasing medical expenses. Under APRIL plans, insurance premiums may be paid annually, semi-annually or quarterly, depending on your policy.
Coinsurance
This is a percentage of medical expenses that you will be responsible for paying if you require medical treatment. Coinsurance can vary from plan to plan, and the higher your coinsurance percentage, the less expensive your annual premium will be.
APRIL offers a fixed co-insurance option of 20% on outpatient visits. This coinsurance will be waived if you visit a medical practitioner within our panel network.
Here is how coinsurance is calculated:

There are other cases in which co-insurance might be applied. For example, hospitalisations, outpatient surgeries, and rehabilitation treatments must be preauthorised prior to treatment, or else a 20% co-insurance fee applies.
Underwriting
Underwriting is the process of assessing risk to offer insurance and set the premium you pay. Underwriters look at several factors, such as your age, gender, occupation (for example, if you work in construction or have other risky jobs), your medical history, and if you have any pre-existing conditions.
If an applicant does not disclose all relevant information on their application form, this could result in them being declined when trying to make a claim later on.
Pre-existing Condition
Before buying a health insurance plan, a pre-existing condition is a health problem you have been diagnosed or treated for, whether successfully or unsuccessfully.
Health insurance companies usually have different ways of covering pre-existing conditions. Minor pre-existing conditions, like a bone fracture for instance, might be covered as standard, without loading to your premium. For more serious conditions, you may be offered different underwriting decisions:
Your condition may be covered, but the insurer will add a loading to your premium,
You may be offered a standard premium, but your condition will be excluded from coverage,
For very serious conditions, like cancer or chronic heart disease, your application may be declined.
This is why it is key for you to apply for health insurance before actually being sick.
Some health insurance plans only cover certain types of pre-existing conditions, while others will cover them all. You should check with your provider to see what they cover before signing up for coverage.
Exclusion
An exclusion is a condition that is not covered under your health insurance policy. It can be related to two things.
First, it can be a specific medical condition or treatment that is excluded from your policy coverage. Some health insurance plans may exclude certain types of care, such as cosmetic treatment, substance abuse treatment, LASIK surgery, or some experimental procedures, for instance.
Second, an exclusion can be determined during the underwriting phase and is linked to a pre-existing condition you declared. For example, if you have a condition like high cholesterol it is likely to be considered as pre-existing and any treatment related to this condition will be excluded from your policy and therefore not covered.
Deductible
A deductible is a fixed amount of money you must pay before your insurance company starts covering you. It can be an amount per policy year and or/per disability, for instance. Usually, the higher the deductible, the more money you will save on premiums. If you are on a budget, adding a deductible to your plan will allow you to pay a more affordable premium. In case of major illness or hospitalisation, you will have to pay your deductible out of pocket but will then be covered up to your annual limit.
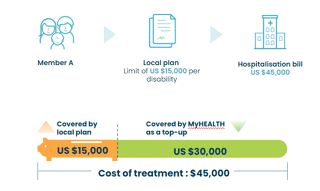
If you already benefit from a basic insurance plan (local plan, company plan…) but would like more comprehensive coverage, you can top up your current policy by adding our MyHEALTH Inpatient Module with a high deductible. In case of treatment, your first insurance plan will cover you up to its limit. Your top-up will then jump in and cover the remaining cost of treatment, ensuring you don’t have anything to pay out of pocket.
For example, let’s say a member has a limit of US$15,000 per disability under his local plan. He is then hospitalised and the bill comes to US$45,000. His existing insurance policy cover him up to its limit of US$15,000, which will apply to his deductible, and APRIL will then cover the remaining US$30,000.
In-network Provider
When you buy a plan with outpatient benefits, you are usually entitled to direct billing services within a network of providers (“in-network providers”). This means that you can enjoy cashless medical services within this network. Instead of charging you, the medical provider will send the bill directly to the insurance company.
Our list of direct billing network list is available at this link. Members may also search for providers part of direct billing networks on their Easy Claim app.
Out-of-Network Provider
An out-of-network provider is any doctor, hospital, or clinic that is not part of your health plan's direct billing network.
Since they do not have a contract with your insurance company, it means they cannot bill them directly for their services and you'll have to pay for the expenses yourself, and then file a claim with your insurer to get reimbursed later.
In conclusion, looking for health insurance can be a confusing process, and there are a lot of factors to consider. But if you're well-informed, you can find the best option for you and your family—which matters most.
What APRIL can do to help
With MyHEALTH, we've delivered insurance solutions that cater to individual needs and provide comprehensive coverage at a fair price.
If you're looking for comprehensive health insurance, our advisers are here to guide you and help you find the plan that suits your needs. Do not hesitate to contact us to discuss your situation in more detail, or click on the button below to get your own quote.
Learn more
- Long-Term International Health Insurance12/2025
Which medical and emergency assistance services are included in my policy?
All APRIL International Care members of one of our Asian plans can benefit from medical and emergency assistance services. Whether you need a second medical opinion while…
- Long-Term International Health Insurance09/2023
Understanding co-insurance: what is it, and how does it work?
Co-insurance is a cost-sharing mechanism on many insurance policies. On MyHEALTH plans, it is an option you can take to help reduce your premium. Here we'll help you understand how…
- Long-Term International Health Insurance09/2023
Breast cancer awareness: signs, symptoms and prevention
According to the Breast Cancer Research Foundation, globally, breast cancer now represents one in four of all cancers in women. Since 2008, worldwide breast cancer incidence has…
- Long-Term International Health Insurance09/2023
What is a pre-existing condition?
Are you planning to purchase a health insurance plan but unsure of the different health insurance terms and what they mean? This article gives a comprehensive guide on a particular…